A New Era in Mental Health Treatment: The Impact of Extended Reality on Neuroscience and Psychiatry
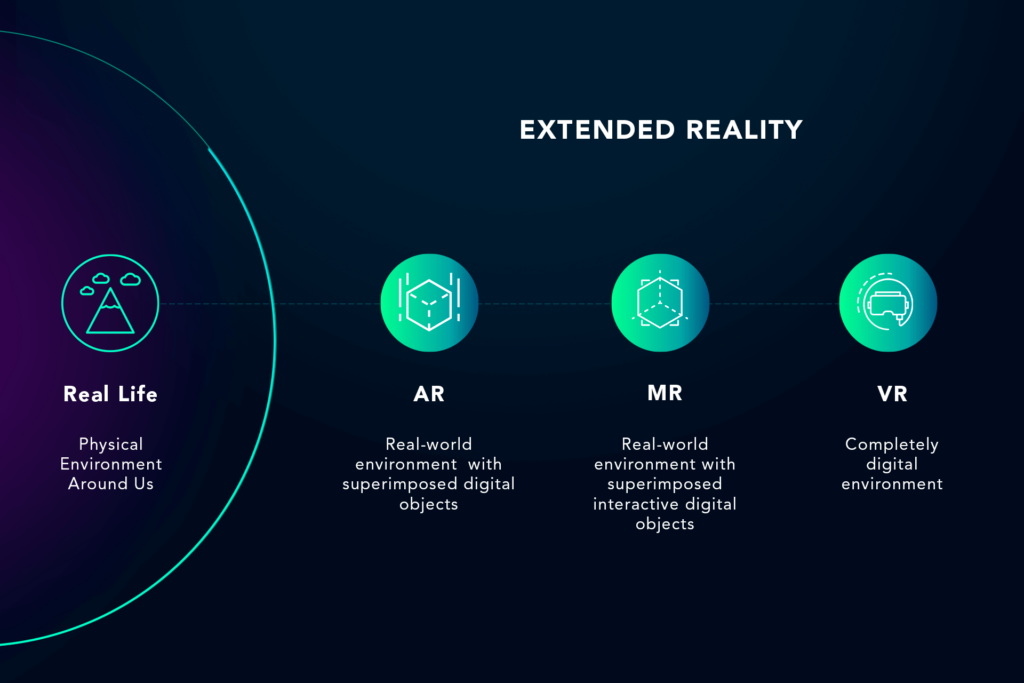
Extended Reality (XR)—a term encompassing Virtual Reality (VR), Augmented Reality (AR), and Mixed Reality (MR)—has moved beyond its initial applications in entertainment and gaming. Today, it has emerged as a groundbreaking tool in neuroscience and psychiatry, reshaping how we study the brain and treat mental health disorders. The immersive nature of XR allows for enhanced understanding and treatment, offering hope to patients suffering from conditions like schizophrenia, post-traumatic stress disorder (PTSD), anxiety, depression, and more.
This article explores how XR technologies are being used in neuroscience and psychiatry, focusing on their potential to revolutionize mental health treatment, improve patient outcomes, and provide new avenues for research.
Understanding Extended Reality in Neuroscience and Psychiatry
Extended Reality (XR) is a broad category that includes various immersive technologies such as Virtual Reality (VR), Augmented Reality (AR), and Mixed Reality (MR). Each of these technologies has a unique way of interacting with the user and can be applied in different settings, including medical and therapeutic applications.
What is Virtual Reality (VR)?
Virtual Reality (VR) immerses users in a completely simulated environment that can be interacted with through specialized equipment like VR headsets and controllers. In VR, the user is placed in a fully virtual world, where they can experience simulated environments, scenarios, and interactions that are not present in the real world. This immersive nature of VR makes it especially valuable in treating psychiatric conditions by offering controlled environments where patients can confront fears, practice coping strategies, or undergo therapeutic interventions.
What is Augmented Reality (AR)?
Unlike VR, Augmented Reality (AR) overlays digital elements onto the real-world environment. Using devices such as smartphones, AR glasses, or headsets, AR enhances the real world with virtual objects, information, or visuals. In neuroscience and psychiatry, AR can be used to visualize brain activity, simulate neurological conditions, or create interactive therapeutic environments for patients.
What is Mixed Reality (MR)?
Mixed Reality (MR) combines elements of both VR and AR, allowing users to interact with virtual objects superimposed on the real world in a way that feels natural and realistic. MR is less commonly used in clinical settings compared to VR and AR but shows great promise in providing more interactive and dynamic therapeutic experiences.
Together, these XR technologies form a cohesive set of tools that can be used to better understand the brain and develop new treatment methods for psychiatric disorders.
How XR Technologies Are Used in Neuroscience and Psychiatry
Neuroscience and psychiatry benefit greatly from XR technologies, as they offer ways to engage patients and clinicians in ways that traditional therapies cannot. XR enables immersive learning and interaction, which can significantly enhance the treatment of mental health disorders.
1. Visualization of the Brain and Neural Networks
One of the most significant applications of XR in neuroscience is the visualization of the brain’s structure and neural networks. Traditional neuroimaging techniques like MRIs and CT scans provide static, two-dimensional views of the brain, but XR technologies can generate 3D models that allow clinicians and researchers to interact with these models in real-time
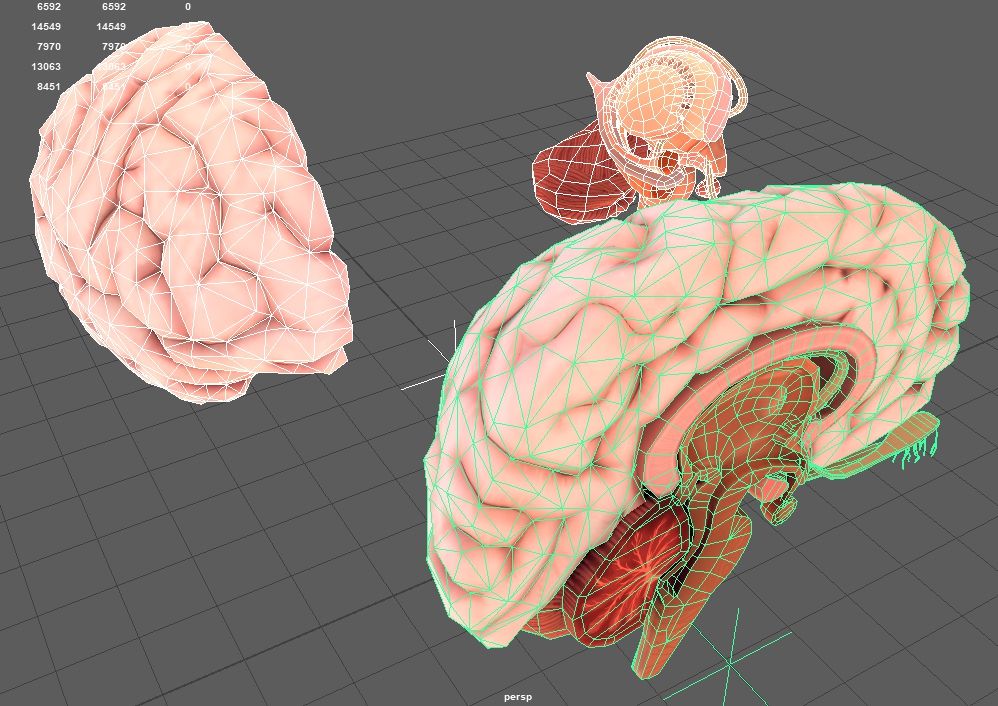
AR for Brain Visualization
AR can be used to project 3D brain models onto physical spaces, allowing medical students and clinicians to interact with these models directly. This can improve understanding of brain anatomy and neural connectivity, especially when studying neurological disorders such as Alzheimer’s, Parkinson’s, or epilepsy.
VR in Neuroscientific Research
In VR, entire virtual brain models can be simulated, enabling researchers to study the progression of neurological diseases in a more dynamic and interactive way. They can manipulate these models to visualize how different brain regions respond to various stimuli, or to observe how diseases like Alzheimer’s affect neural pathways over time.
2. Surgical Planning and Navigation
In neurosurgery, precision is paramount. XR technologies are helping surgeons plan and perform operations with greater accuracy, reducing risks and improving patient outcomes. AR is particularly beneficial in preoperative planning, while VR is useful for surgical training and practice.

AR for Surgical Precision
Surgeons can use AR to overlay critical information, such as MRI or CT scans, directly onto the patient’s anatomy during surgery. This technology helps surgeons pinpoint exact areas of interest, such as tumors or damaged tissue, and navigate the brain more precisely.
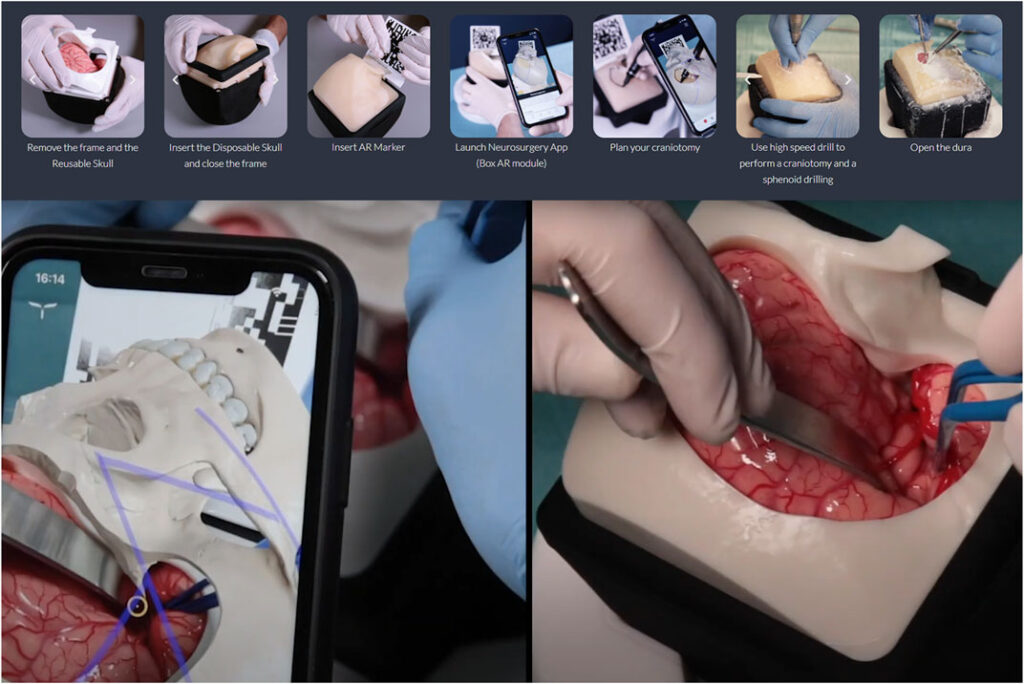
VR for Surgical Training
VR is being used in medical training to simulate complex surgeries. Surgeons can practice procedures in a fully immersive environment, which allows them to gain experience without the risk of real-life complications. This approach helps build confidence and competence before performing actual surgeries.
XR in Treating Psychiatric Disorders
Psychiatric disorders often involve disruptions in perception, cognition, and behavior, making them difficult to treat with traditional methods. XR technologies offer new ways to treat these disorders by immersing patients in virtual environments that allow them to confront and reframe their fears and anxieties in a safe and controlled setting.
1. Exposure Therapy with VR and AR
One of the most well-established uses of XR in psychiatry is exposure therapy, which helps individuals face their fears in a gradual and controlled manner. By simulating real-life situations, VR and AR provide a safe environment for patients to experience anxiety-provoking scenarios without the actual risks involved.

VR for Anxiety and PTSD
Patients with conditions like PTSD, social anxiety, or phobias can undergo virtual scenarios designed to trigger their fears in a controlled manner. For example, veterans with PTSD may be exposed to virtual warzones, allowing them to confront trauma-related triggers while under the supervision of a trained therapist. This exposure helps them reframe their trauma responses and gradually reduce the emotional impact of the memory.
AR for Gradual Exposure
AR can offer gradual exposure by superimposing virtual threats onto the real world. For example, individuals with a fear of heights could experience AR simulations of high places while standing in a safe environment, such as their home or therapy office. This allows them to confront their fear at their own pace.
2. Cognitive Behavioral Therapy (CBT) with XR
Cognitive Behavioral Therapy (CBT) is one of the most effective treatments for a variety of psychiatric disorders, including depression, anxiety, and OCD. XR can enhance CBT by providing interactive and immersive experiences that engage patients in therapeutic exercises.
VR in CBT
In VR-based CBT, patients interact with virtual environments designed to challenge negative thought patterns. For instance, patients can practice social interactions in virtual settings, helping them build confidence in social situations that may trigger anxiety or depression.
AR in CBT
AR can supplement CBT by providing real-time feedback during therapeutic exercises. Patients can interact with virtual objects or visualizations, which help them process emotions or practice coping mechanisms in response to negative thoughts or feelings.
3. Mindfulness and Stress Reduction with XR
Mindfulness practices are known to improve mental health by helping individuals manage stress, anxiety, and emotional distress. XR technologies can be used to create immersive environments that promote relaxation and mindfulness.
VR for Mindfulness
Virtual environments, such as beaches, forests, or peaceful gardens, can help patients relax and reduce stress. These calming settings can be used alongside breathing exercises or guided meditation to promote mindfulness and emotional regulation.
AR for Stress Reduction
AR can overlay calming visuals onto real-world settings, such as serene nature scenes or gentle rain sounds. This approach helps patients take short breaks during stressful moments and experience a sense of calm in their everyday environments.
Case Study: Freeman’s Work on Schizophrenia and Virtual Reality
Professor Daniel Freeman, a clinical psychologist at the University of Oxford, has conducted groundbreaking research exploring the use of virtual reality (VR) in treating schizophrenia, specifically targeting symptoms of paranoia and social withdrawal. These symptoms, which often severely impair daily functioning and interpersonal relationships, can be challenging to address with traditional therapeutic methods. Freeman’s research represents a pivotal step in leveraging immersive technologies for mental health interventions.
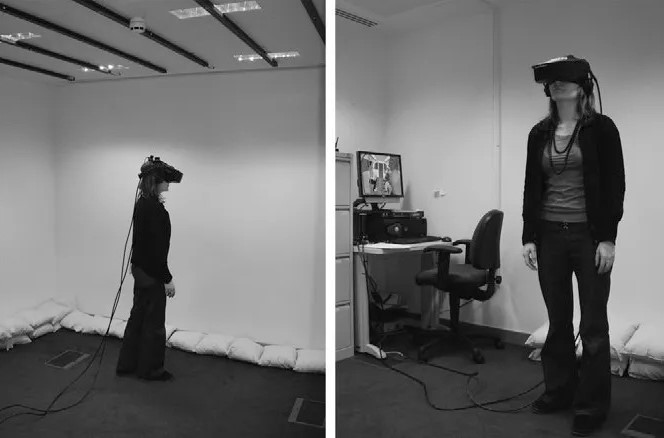
The Setup
Freeman’s research involved creating VR simulations of common social situations that individuals with paranoia might find distressing. These simulations included environments like public transportation, busy shopping centers, and elevators, where the participants could interact with avatars designed to provoke paranoid thoughts.
Participants wore VR headsets that immersed them in these scenarios, while therapists provided real-time support, helping patients reframe their thoughts and manage their anxiety.
The Results
The results of Freeman’s study were impressive. Many participants showed significant reductions in paranoia and reported increased confidence in real-world social interactions. For example, one participant described the experience as transformative, realizing that the avatars in the simulation were not out to harm them.
Follow-up assessments revealed that the improvements were sustained over time, with participants maintaining reduced paranoia and improved functioning months after the therapy ended. This case study highlights the potential of VR in bridging the gap between the safety of clinical therapy and real-world challenges.
Benefits of XR in Neuroscience and Psychiatry
XR technologies offer numerous benefits in neuroscience and psychiatry:
- Personalized Therapy: XR tools can be customized to suit the individual needs of each patient, making therapy more effective.
- Accessibility: Mobile AR and VR applications allow patients to access therapeutic tools from the comfort of their homes, reducing the need for frequent clinic visits.
- Engagement: The interactive and immersive nature of XR motivates patients to actively participate in their treatment, especially among younger or more resistant patients.
- Reduced Stigma: XR-based therapies feel less clinical, which may help reduce the stigma associated with seeking mental health care.
Benefits of XR in Neuroscience and Psychiatry
Despite its promise, XR in mental health care faces challenges:
- Cost and Accessibility: Advanced XR systems are expensive, which could limit their adoption, especially in resource-limited settings.
- Technological Limitations: Current XR devices may need improvements in resolution, processing power, and user comfort.
- Therapist Training: Clinicians need proper training to integrate XR tools into their practices effectively.
Looking ahead, the future of XR in mental health will likely see greater integration with artificial intelligence (AI). AI can be used to personalize and adapt XR-based treatments in real-time, ensuring that patients receive the most effective care.
Conclusion
Extended Reality is poised to revolutionize the field of neuroscience and psychiatry. By providing immersive, interactive experiences that engage both patients and clinicians, XR technologies are reshaping how mental health disorders are treated and understood. From exposure therapy to cognitive behavioral interventions, XR offers exciting new possibilities for improving mental health care outcomes. As these technologies continue to evolve, their integration with AI and other advancements will unlock even more potential, ultimately transforming the future of psychiatric treatment and neuroscience research.

Maryam Salman
A-levels student | The Lahore Lyceum
Maryam is an A-levels student hailing from Lahore, Pakistan who is passionate about Tech-Driven movements, Human-Computer Interaction, and Psychiatry; You will often find her writing about how these fields intersect within the mundane tasks of life. She has been an avid reader since age five, and when she's not writing or reading, she finds joy in baking—it’s her favorite way to relax!

